Tibia fractures are among the most frequent long bone injuries treated in hospitals, and the method used to stabilize them often decides how quickly a patient returns to daily life. For years, infrapatellar intramedullary nailing has been the standard choice. It has worked reasonably well, but it comes with certain drawbacks: knee discomfort, alignment problems in tricky cases, and slower early mobilization. That’s why more hospitals today are considering, and often adopting, the suprapatellar nailing system.
Now, making a switch in surgical instruments isn’t simple for any clinical team. Questions come up: Do results justify the change? Is it cost-effective? Will surgeons adapt quickly to the newer method? These are valid concerns, but when you look closer at both the clinical outcomes and the patient experience, the case for adopting suprapatellar nailing becomes very strong.
Better Alignment From the Start
One of the major issues with infrapatellar nailing is alignment. When the knee has to be bent for entry, the tibia is placed under unnatural tension. Even a perfectly skilled surgeon may find the fracture edges shifting, especially in proximal third fractures. Malalignment—angular or rotational—can show up later on X-rays and, more importantly, in the patient’s gait.
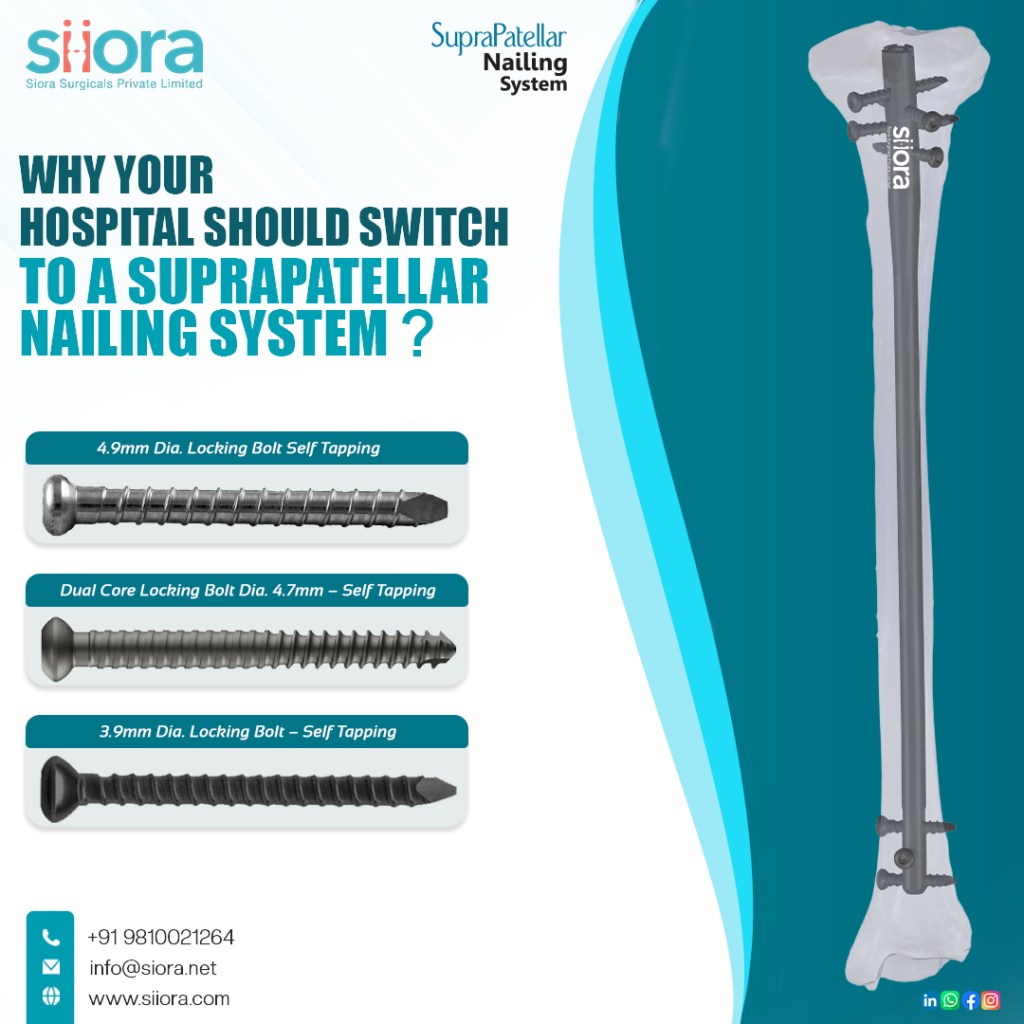
With suprapatellar nailing, the entry is made above the knee cap while the leg remains straight. In simple terms, this means the bone is kept in its natural line. Surgeons can see and maintain that alignment under fluoroscopy with far less struggle, which makes accurate fixation more predictable. For hospitals, that translates into fewer revision cases and better long-term outcomes.
Reduced Postoperative Pain
Anterior knee pain is one of the most common complaints after infrapatellar nailing. The standard approach involves manipulating or splitting the patellar tendon, which can irritate tissue and cause lingering discomfort. Patients often voice this pain during follow-ups, and managing it adds time to rehabilitation.
The suprapatellar system avoids the patellar tendon entirely. Entry is achieved through a protective sleeve above the kneecap, shielding the cartilage surface of the joint. Patients benefit with less postoperative discomfort around the knee, which keeps them more willing to participate in physiotherapy. And as any orthopedic nurse will tell you—that willingness makes a big difference in recovery speed.
Faster Rehabilitation and Shorter Stays
Every hospital today is under pressure to shorten inpatient stays while still ensuring quality care. Early mobilization is key to that balance. With suprapatellar nailing, patients can often begin partial weight-bearing or physiotherapy sooner compared to the traditional system. Less pain, combined with better alignment, simply makes it easier for them to move the limb.
For administrators, the benefits show up as reduced rehabilitation costs and higher patient satisfaction scores. For surgeons, it is satisfying to see tangible improvement in recovery speed without compromising safety.
Surgeon Comfort and Workflow
It is easy to think only of patient benefits, but surgeon comfort during the procedure must also be counted. Performing nailing in a knee-flexed position for long periods can be tiring and awkward. Suprapatellar technique, with the limb extended, offers a more ergonomic working posture. Fluoroscopic imaging is also easier with the leg straightened. What this really means is that operations run more smoothly, and teams may finish cases faster with less intraoperative strain.
Looking at the Bigger Picture
Yes, adopting a suprapatellar system involves training and trauma instrument investment. But hospitals that have made the shift often note that the learning curve is not steep, and the protective sleeves used in the procedure provide confidence even for surgeons who are newer to the approach. The payoff is seen in fewer complications, fewer complaints of knee pain, and consistently improved fracture alignment.
Final Word
So, why should your hospital switch? Because patient expectations are rising, and so are the pressures on doctors to deliver faster recovery with fewer complications. Suprapatellar nailing addresses both sides. By easing alignment, protecting the knee, and streamlining rehabilitation, it delivers a modern standard of care that patients notice and appreciate.
For hospitals aiming to stay ahead in orthopedic excellence, the question may not be if you will adopt the suprapatellar system, but when.